AI Chat Bot
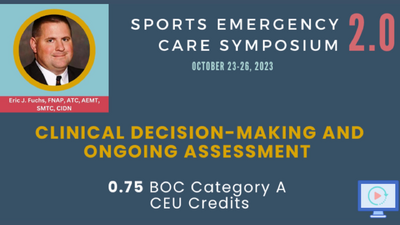
Clinical Decision-Making and Ongoing Assessment › Learning Material
Presentation (Video)
Updated Jan 22, 2024
Copyright © 2025 Action Medicine Consultants, LLC
___MESSAGE___
___MESSAGE___